Spotlight 1/4
Hospital security protocols
Patient Ombudsman has seen an increase in the number of complaints describing negative interactions between health care providers, patients and their caregivers.
The COVID-19 pandemic continues to widen the cracks in Ontario’s health care system.
Staffing shortages, COVID restrictions and service delays, together with the fatigue and trauma arising from the pandemic, have contributed to increased tension, frustration and occasionally violence in health care settings. Patient Ombudsman has seen an increase in the number of complaints describing negative interactions between health care providers, patients and their caregivers.
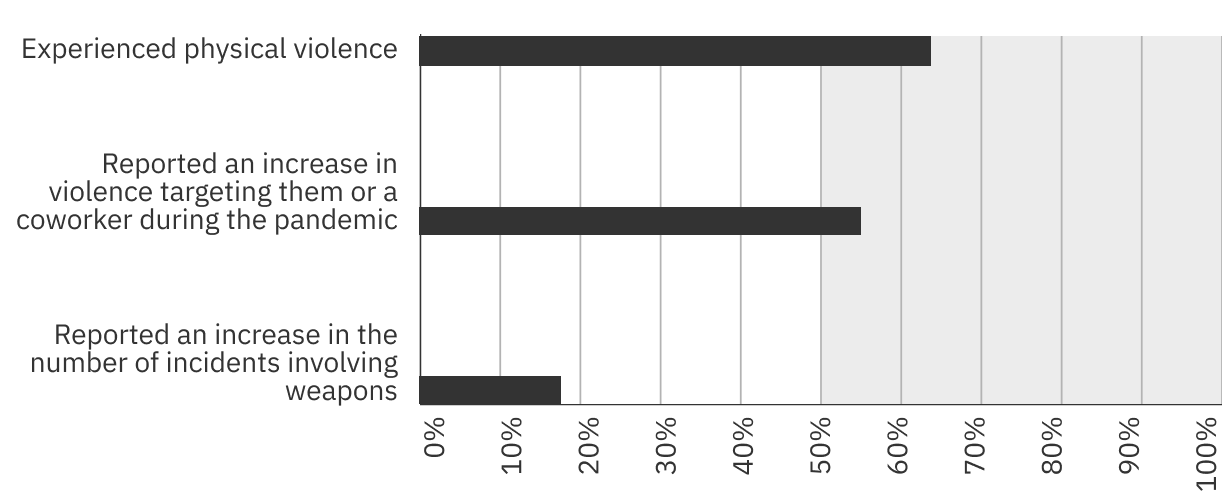
A recent poll of more than 2,000 health care workers by the Canadian Union of Public Employees1 revealed that more than half had either experienced or witnessed an increase in violence since the beginning of the pandemic. Sixty-three per cent of respondents reported they had experienced physical violence at their workplaces and 18% reported an increase in the number of incidents involving weapons since March 2020.
2,000 health care workers polled by the Canadian Union of Public Employees1
Presence of this issue in 2019-2021
In its last annual report, “Courage , Compassion, Clarity: Informing change in a time of crisis”, Patient Ombudsman highlighted the growing number of patients and caregivers reporting the involvement and use of force by hospital security guards.
Recommendations
Patient Ombudsman identified this as an area needing more attention and suggested that, at a minimum, health sector organizations should:
Have a use of force policy that is sensitive to the patient populations and cultures served.
Ensure all security personnel receive de-escalation training and recognize that use of force is a last resort.
Ensure policies, procedures and training for security encompasses unconscious bias and supports the needs of diverse persons using the hospital.
Document and review all incidents that involve the use of force against patients and visitors to ensure that policies and procedures were followed and identify opportunities for improvement.
Optimize the use of technology in reviewing use of force incidents, for example, security video or implementing body-worn cameras.
The issue in 2021/22
In 2021/22, 98 of the 2,005 complaints about public hospitals included descriptions of negative interactions with hospital security as an element of the complaint – 5% of complaints involving hospitals. Twenty-two of the complaints alleged assaults or physical harm. Several complainants reported being restrained in an unsafe manner that is inconsistent with the standard training for security guards (for example, with a security guard’s knee on their neck or back), that could cause severe injury or death. Most interactions with security occurred in emergency departments, on mental health units and at screening points for entry to hospitals.
Additional concerns
Patient Ombudsman has identified several additional concerns in reviewing complaints about aggressive interventions by security. These include:
- Patient relations representatives often defer to hospital security and do not take an active role in reviewing these complaints.
- Health sector organizations often lack a clear, standardized process for investigating incidents involving hospital security guards. Organizations often failed to review or retain security video, and documentation sometimes needed to be reconstructed for the purpose of Patient Ombudsman’s review.
- Hospitals were sometimes reluctant to share information with patients or their caregivers about who was involved in the incident.
- Complaints about the conduct of individual security guards were not routinely shared with the Ministry of the Solicitor General, the licensing body for security guards, for review.
- Patients reported being traumatized by these incidents and expressed discomfort when security guards were present or assisted when the patient’s clothing was removed.
Our recommendations
Patient Ombudsman was encouraged that some hospitals undertook comprehensive reviews of incidents involving security and were implementing policy and process improvements. A few hospitals were actively considering a requirement for security guards to wear body cameras.
Building on the suggestions from the last annual report, Patient Ombudsman makes the following additional suggestions for incidents involving hospital security:
- Ensure there are comprehensive policies and procedures for reviewing incidents involving hospital security, particularly when force is used to restrain or evict patients, caregivers or visitors. The policies and procedures should define the role of patient relations in reviewing the complaints.
- Ensure all incidents are fully documented and preserve relevant evidence, including security video.
- Concerns about the conduct of individual security guards should be referred to the licensing body, the Ministry of the Solicitor General, for review.
- If health sector organizations cannot or will not provide the name of a security guard when requested by patients or caregivers, the guard’s license number is sufficient for the patient or caregiver to make a complaint to the Ministry of the Solicitor General.
- When possible, health sector organizations should make efforts to gender match security guards with patients and offer referrals to victim assistance organizations when patients report feeling traumatized.
